Medicaid Expansion
One of the most important and controversial provisions of the Affordable Care Act is the expansion of health coverage to low-income families through the Medicaid program.
Federal matching funds
States can receive federal matching funds for covering additional low-income individuals and families under Medicaid for whom federal funds were not previously available.
Medicaid expansion was intended to be national, but the June 2012 Supreme Court ruling essentially made it optional for states.
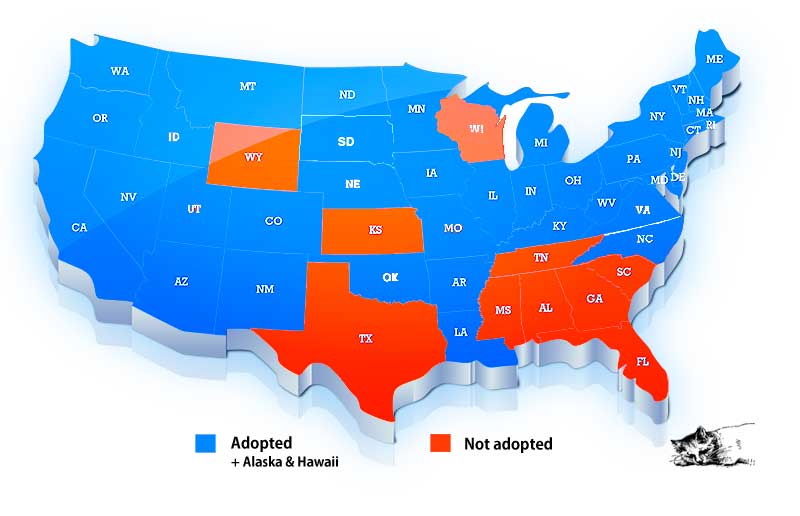
► 41 states, including the District of Columbia have taken advantage of federal funds and expanded their Medicaid programs to provide health coverage to more of their residents.
Initially states could receive 100% federal funding for the first three years to support this expanded coverage, phasing to 90% federal funding in 2020 and future years.
States that delayed expansion, like South Dakota, will not receive 100% funding but can receive 90% funding.
♦ The map is slowly changing. Ten states still have not expanded Medicaid under the Affordable Care Act.
When the question of Medicaid expansion has been put on the ballot, it has passed every time.
Unfortunately, Republican controlled legislatures do not want their citizens to vote on this issue.
♦ March 2, 2023 — North Carolina's legislative leaders announced an agreement had been reached to expand Medicaid.
The legislation passed as a part of the state budget but the governor did not sign it. He didn't do anything and it became became law.
It's estimated that more than 600,000 people in North Carolina are newly eligible for Medicaid under the expanded eligibility rules.
Medicaid is not Medicare
Medicaid is intended to help the poorest and most vulnerable of our population. Medicaid provides health coverage for low-income people, families and children, pregnant women, the elderly, and people with disabilities.
♦ 74% of Americans have a favorable view of Medicaid, according to a Kaiser Family Foundation survey. It is likely that this favorable view is because a large number of senior citizens rely on Medicaid to help cover nursing home care.
Before the healthcare law, Medicaid didn’t cover low-income adults without dependent children unless they were pregnant, age 65 or older, or had serious disabilities.
Beginning on January 1, 2014, all children, parents and childless adults who are not entitled to Medicare and who have family incomes up to 133% of the Federal Poverty Level will become eligible for Medicaid — in states that expanded their Medicaid programs.
♦ As of September 2023, close to 88 million individuals were enrolled in Medicaid and CHIP in the 50 states and the District of Columbia.
Medicaid enrollment is projected to decline to 81.1M by 2025 as states disenroll beneficiaries no longer eligible for coverage because the COVID-19 public health emergency (PHE) has ended.
• Of the 88 million total, just under 40 million were children enrolled in CHIP. This represents about 46.1% of total Medicaid and CHIP enrollment.
♦ Medicaid is the primary payer for long-term care. Medicaid covers 6 in 10 nursing home residents.
In 2022, Medicaid spent close to 806 billion dollars. Of this amount about 37% goes to covering long-term care such as nursing homes.
♦ Of this 806 billion, the federal government paid about 69% and 31% was financed by states.
In 2022, the Federal government authorized a 6.2% increase in the federal Medicaid match rate. The additional funds were retroactively available to states beginning January 1, 2020.
The additional funds will continue through the last day of the calendar quarter in which the public health emergency ends. The federal COVID-19 emergency declaration ended on May 11, 2023.
Someone loses
People living in states that chose not to expand their Medicaid programs lose.
♦ An estimated 2.2 million people fall into the so-called "coverage gap" — too poor to qualify for subsidies to use at the marketplaces to buy insurance but lacking access to Medicaid because they live in a state that refused Medicaid expansion.
Note — Because of the way Medicaid eligibility is calculated, the qualifying level turns out to be 138% of the Federal Poverty Level. In addition, a few states use a different income limit.
Medicaid primarily uses Federal tax dollars but is administered by the states. Some states also supplement their Medicaid programs with State funds. Because the states have considerable leeway in how they run their programs there can be different requirements depending upon the state you live in.
♦ It is important to note that per CMS guidance, there is no deadline for states to implement the Medicaid expansion.
Federal funding was made available to cover 100% the costs through 2016, with funding gradually dropping off until it reaches 90%.
In 2020, the federal share dropped to 90%. Future years will continue at 90%.
• Wisconsin's governor wants to expand coverage to more people. But Wisconsin's republican-controlled legislature won't go alone.
• Georgia is trying to slide through a twisted version of Medicaid expansion before the Biden administration put the brakes on their plans.
In November 2019, Governor Kemp presented a brief outline that suggested his plan would only cover up to 50,000 people. In Georgia an estimated 408,000 people make less than the Federal Poverty Level but do not qualify for Medicaid.
In December 2021, Georgia's Medicaid waiver was denied.
In August 2022, a Federal Court vacated CMS's rescission putting the waiver back in play.
Voter initiatives
♦ Citizens in several states, including Idaho, Utah and Nebraska were able to beat back strong Republican opposition to voter initiatives to put the question of Medicaid expansion to a vote.
→ Idaho: Medicaid expansion passed by a vote of 60 to 40. In April 2019, Idaho's legislature passed legislation to make changes to the Medicaid expansion approved by the voters. They wanted to limit expansion up to 100% of FPL. This failed and expansion proceeded on January 1, 2020 up to 138% of FPL. The Governor and the legislature continues to push for a work requirement. The Biden Administration rejected all work requirement waivers in 2021. The issue is now tied up in the courts.
→ Utah: Medicaid expansion passed by a vote of 54 to 46. Medicaid was to be expanded by April 1, 2019 but the Governor and legislature had other plans. Medicaid expansion was pushed out to January 1, 2020 with a work requirement rule added. December 23, 2019, CMS approved Utah's waiver request to include work requirements but did not approve the request to cap enrollment. Medicaid expansion up to 138% of FPL became effective on January 1, 2020. In August 2021, the Biden Administration withdrew Utah's work requirement waiver.
→ Nebraska: Medicaid expansion passed by a vote of 53 to 47. Nebraska's legislature is going all out to delay expansion. It now looks like two years after voters approved the ballot initiative they may finally get something. Expansion is scheduled to start on October 1, 2020. The state continues to submit waiver requests. On October 20, 2020, CMS approved Nebraska's waiver with implementation of some waiver elements to begin on April 1, 2021 and others (including the work requirement) to follow one year later. August 17, 2021 the state withdrew its waiver request. Medicaid expansion with full benefits started from October 1, 2021.
→ Montana: A ballot initiative to generate funding to continue Medicaid expansion failed by a vote of 53 to 47. Medicaid expansion was going to end in July 2019 but Montana lawmakers reauthorized the expansion for six more years on the condition that there be a work requirement. Waivers were submitted on August 30, 2019 requesting a work requirement and an increase in premiums. The Biden Administration reject both waivers.
→ Ohio: Republican Mike DeWine was elected governor. He is opposed to the Medicaid expansion put in place by outgoing Republican Governor John Kasich. Ohio received permission in March 2019 to add a work requirement. It was to be implemented in January 2021. In August 2021, the Biden Administration withdrew the work requirement waiver .
Power changed hands
♦ Maine voters approved expansion in 2017, but their Republican governor refused to do anything. Governor Janet Mills (D) took office in January and immediately put an end to the stonewalling.
♦ May 30, 2018 The Virginia General Assembly approved Medicaid expansion as a part of a budget bill. Governor Northam signed the budget into law on June 7th. Medicaid expansion became effective on January 1, 2019.
Governor Northam's hands were tied by the Republican controlled legislature which demanded that work requirements be included. Waivers for work requirements were sought but then in 2019 the legislature flipped to the Democrats and waivers were soon cancelled.

